Newly Recognized Pathway Could Protect People with Diabetes from Hypoglycemia
“Delta” Cells, a Longstanding Medical Mystery, Could be Key
A new study by the University of California, Davis, shows how cells work together to avoid a sudden drop in blood sugar. Understanding these feedback loops could improve the lives of people with diabetes and help them avoid dangerous hypoglycemia.
The work was published Sept. 16 in Proceedings of the National Academy of Sciences.
People with diabetes must contend with the long-term risks of high blood sugar, such as blindness, kidney failure, and loss of circulation in the legs, which can lead to amputation. But many people with this condition also face a more immediate danger that can strike without warning: blood sugar that drops dangerously, which can cause unconsciousness. This can occur due to the insulin and other medications that they take.

“Your body tissues are essentially starving when this happens, especially the brain,” said Mohammad Pourhosseinzadeh, an M.D./Ph.D. student at UC Davis, who recently graduated from the Biochemistry, Molecular, Cellular and Developmental Biology Graduate Group. “If you don’t get quick medical attention, you can eventually go into a coma and die.” People who experience severe hypoglycemia may also be at increased risk of dying from heart disease and other causes.
Pourhosseinzadeh, working with Mark Huising, professor in the departments of Neurobiology, Physiology and Behavior and of Physiology and Membrane Biology, was part of a team that has discovered an important link in how the body protects itself from hypoglycemic emergencies.
It’s well-known that people with diabetes don’t produce enough insulin, the hormone that prevents our blood sugar from rising too high. “But the body’s mechanism for preventing blood sugar from dropping too low is also impaired in diabetes,” Huising said.
The new discovery reveals a potential strategy for treating this dangerous aspect of diabetes. It also helps to solve a longstanding medical mystery.
Mystery cells and mystery hormone
Insulin is produced by tiny clumps of cells in the pancreas, called the Islets of Langerhans. These islets contain at least five types of cells that are visible under a microscope: the alpha, beta, gamma, delta and epsilon cells. By the 1920s, scientists understood that insulin is produced by the most numerous of these, the beta cells, which make up roughly half of each islet.
In type I diabetes, the beta cells are destroyed, leaving a person with no insulin. In type II diabetes, the beta cells are present but produce too little insulin. As a result, many people with diabetes have to inject insulin to keep their blood sugar from rising too high. Some people also take medications that stimulate their sluggish beta cells to make more insulin. For decades, scientists mainly studied the beta cells, hoping to improve these treatments.
“The delta cells were mostly ignored,” said Huising. They made up only 5% of the islet cells, and no one knew their function.
When a person’s blood sugar rises, the 500 or so beta cells in each islet begin to pulse in unison, squirting insulin into the bloodstream for several minutes, then pausing before putting out another pulse of insulin. With each insulin pulse, the beta cells also secrete a little of another hormone, urocortin-3.
In 2015, Huising discovered that urocortin-3 causes delta cells to release a hormone called somatostatin, which in turn tells beta cells to pause secretion of insulin.
“The delta cells are tapping the brakes on insulin production,” Huising said.
In 2024, the team showed that in mice without delta cells, blood sugar stayed consistently about 20% below normal, because they could not produce somatostatin in response to urocortin-3. People with diabetes have reduced levels of urocortin-3 – and hence, altered levels of somatostatin in their pancreatic islets. The mouse study suggested that this is one important reason they are susceptible to hypoglycemia.
Islet cells sing in unison
To Huising and Pourhosseinzadeh, it suggested that medical treatment for diabetes could be improved by finding a way to restore the function of urocortin-3. This would allow delta cells to keep closer tabs on insulin production. The new study lays out possibilities for doing this.

Pourhosseinzadeh found that when the beta cells begin putting out pulses of insulin, the delta cells pulse to the same rhythm, as calcium levels in all the cells rise and fall in unison. These calcium pulses spread from beta cells to neighboring delta cells through tiny electrical connectors called gap junctions composed of protein called connexin 36. This is similar to the way that heart cells contract in unison.
If Pourhosseinzadeh disrupted those electrical junctions between the beta and delta cells, the delta cells no longer responded to tamp down insulin production — even when they received urocortin-3.
“You have a 1-2 punch,” he said. “The rapid signal through gap junctions primes the delta cells, gets them ready to respond. Then after a delay of 30 seconds or so, the urocortin-3 signal turns that response up,” and the delta cells release somatostatin, pausing insulin production.
Restoring this coordination between beta and delta cells could improve the lives of people with diabetes, by preventing severe bouts of hypoglycemia, Huising said: “We are actually studying how this 1-2 punch can be utilized to make the existing drugs work better.”
Additional authors on the new paper include, at UC Davis: former graduate students Jessica Huang, Donghan Shin and Ryan Hart; and former undergraduate students Luhaiza Framroze, Jaresley Guillen, Joel Sanchez, Ramir Tirado and Kelechi Unanwa.
Huising’s research is funded by the National Institutes of Health and the UC Davis Training Program in Molecular and Cellular Biology.
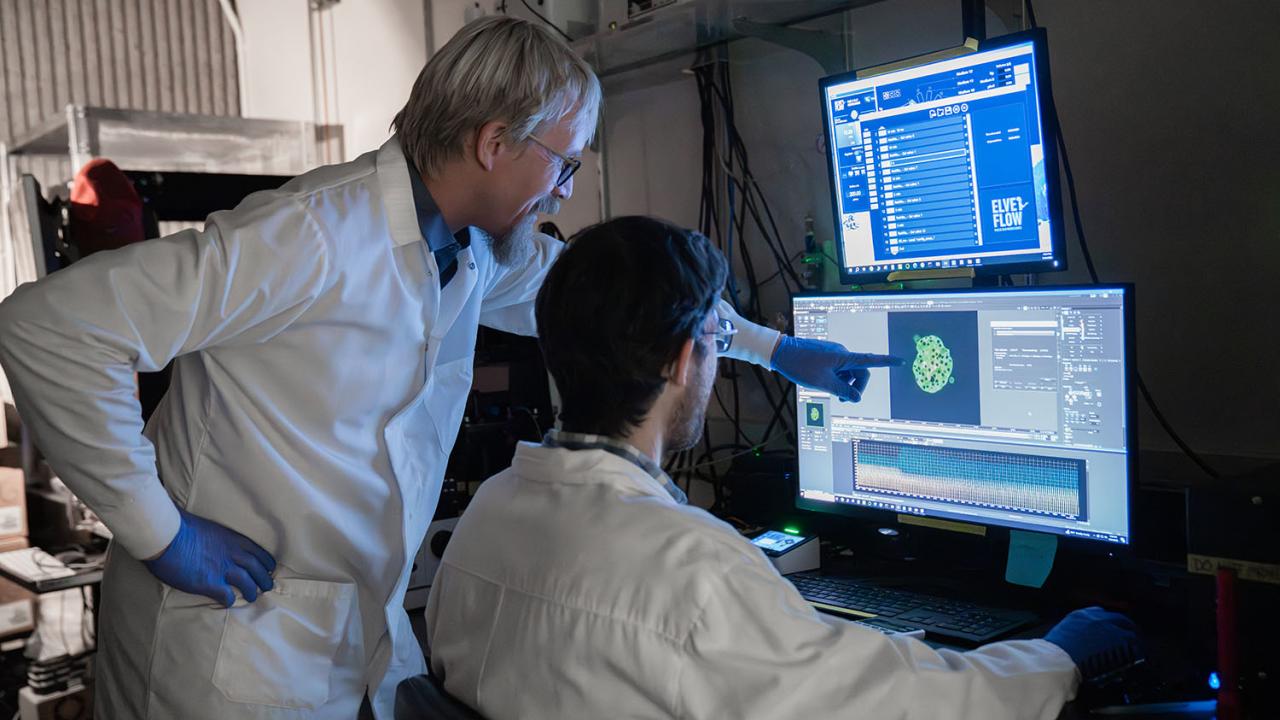
The research documented utilized advanced facilities at the UC Davis Flow Cytometry Core.

Media Resources
- Huising Lab
- Heterogeneity in the coordination of delta cells with beta cells is driven by both paracrine signals and low-density cx36 gap junctions (Proceedings of the National Academy of Sciences 2025)
- Douglas Fox is a freelance science writer based in the Bay Area.
